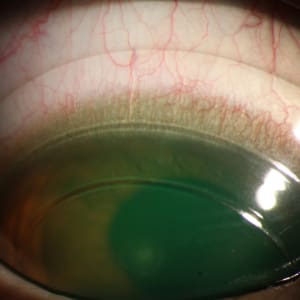
What is Keratoconus?
According to the American Optometric Association, KERATOCONUS is a condition that occurs when the normally round cornea (outer, transparent part of the eye) becomes thin and cone-shaped. This irregularity prevents the light entering the eye from being focused correctly on the retina which then causes distortion and blurring of vision.
“Growing up, parents would notice that there was a need to change the prescription of their child more frequently.
It seemed that the prescription was always taken incorrectly, and your child’s astigmatism and nearsightedness got higher with each vision examination. Then eventually, the prescription was not enough to provide the patient with the usual coveted 20/20 perfect vision with their glasses or conventional contact lenses. And it is because a person with keratoconus would usually not achieve the 20/20 vision, many would mistake the condition as a simple amblyopia or lazy eyes.
A keratoconic cornea becomes irregular thus the astigmatism created is also irregular, causing conventional glasses or contact lenses to be unsuitable for correction.”
How many people have Keratoconus?
Originally, keratoconus was deemed rare, having an incidence of 1:2000 during a published study in 1986. However, recently, a study involving the population in the Netherlands resulted in a prevalence of 1:375 of keratoconus in the general population. Over the years, we have seen a greater amount of keratoconus referrals and realized that indeed this condition is not at all rare, with a pool of patients being detected during the screening for refractive surgery consults.
How Keratoconus can be managed?
Corneal Collagen Cross Linking
Usually, the protocol in managing keratoconus patients would include a discussion about corneal collagen cross-linking that aims in controlling the worsening of the disease. If there is an indication that the keratoconus of the patient is progressing, collagen cross-linking may be performed. In collagen cross-linking, riboflavin (vitamin B2) is administered in conjunction with ultraviolet A which leads to biomechanical stiffening of the cornea. It was shown that this procedure flattens the cornea by about 2 Diopters and may improve vision to about 2 lines or 10 letters. Some patients would delay this procedure, but note that there is a minimum cut-off corneal thickness for the surgeon to still allow to do the procedure for safety purposes.
Intrastromal Corneal Ring Segments
These are small, crescent-shaped plastic rings that are placed in the deep, peripheral corneal stroma in order to flatten the cornea. They are made of polymethylmethacrylate (PMMA). This too may flatten the cornea to about 2 Diopters, and may improve uncorrected vision to about 2 – 4 lines as noted in different studies. This is not a must in the keratoconus management, however, it may be indicated if contact lenses cannot be fitted due to the very steep cornea.
Corneal Transplants
In the worst cases, corneal transplantations are considered. Only about 10-28% of keratoconus patients would need corneal transplantation to improve their vision. Corneal transplant is only indicated if vision cannot be improved anymore with contact lenses and if lenses are intolerable already. The average long-term graft survival is nearly 20 years. This means that a young patient can have more than one corneal transplant in a lifetime. Vision with correction will definitely be improved however note that uncorrected, patient may still have astigmatism. If your keratoconus was severe before the transplantation, it is possible for you to see a dramatic change in your uncorrected vision. Some patients may be happy with their uncorrected vision post the transplant, but most would still need contact lenses to achieve good vision.

Special Designed Contact Lenses
In general, to attain good vision, specially designed contact lenses would still be needed after the collagen cross-linking, intrastromal ring implantation and corneal transplant. This is why, before considering corneal transplants, all contact lens options should be exhausted to see if vision can still be satisfactory with them. Most often than not, one can achieve good vision with contact lenses. Attaining a 20/20 vision is not impossible but it is also not the default. It all depends on the severity of the condition and if the cornea does not have scars.
What are the Different Types of Contact Lenses for Keratoconus?
Special contact lenses include small GP (gas permeable) lenses, large GP lenses (scleral lens), soft customized contact lenses and hybrid contact lenses. Small gas permeable lenses, hybrid contact lenses and Keraosft IC soft customized contact lenses are indicated for mild to moderate cases, while scleral contact lenses are often used for patients who cannot tolerate small gas permeable lenses and for all stages of keratoconus.
Here is the link https://goldheartoptical.com/scleral-lens-and-kerasoft-ic-fitting to know more about the different types of contact lenses for keratoconus and to get a copy of the FAQs on Keratoconus.
References:
- Javadi M. A., Motlagh B. F., Jafarinasab M. R., et al. Outcomes of penetrating keratoplasty in keratoconus. Cornea. 2005;24(8):941–946. doi: 10.1097/01.ico.0000159730.45177.cd.
- Sykakis E et al.Corneal Collagen Cross-linking for treating keratoconus. Cochrane Database Syst Rev. 2015 Mar 24;93): CD010621.
- Wollensak G, Spoerl E, Seiler T. Stress-strain measurements of human and porcine corneas after riboflavin-ultraviolet-A induced cross-linking.Journal of Cataract and Refractive Surgery. 2003;29(9):1780-1785.
- Zadnik K, Money S, Lindsley K.Intrastromal corneal ring segments for treating keratoconus. Cochrane Database Sys Rev. 2019 May 14.
- Kelly T, Williams KA, Coster DJ, Australian Corneal Graft Registry. Corneal Transplantation for Keratoconus: A Registry Study. Arch Ophthalmol.2011;129(6):691–697. doi:10.1001/archophthalmol.2011.7
- Kennedy RH, Bourne WM, Dyer JA, 1986. A 48-year clinical and epidemiologic study of keratoconus. Am. J. Ophthalmol101, 267–273.
- Godefrooij DA et al.Age-specific Incidence and Prevalence of Keratoconus: A Nationwide Registration Study. Am J Ophthalmol. 2017 Mar; 175:169-172.
- Grentzelos MA, Kounis GA, Diakonis VF, Siganos CS, Tsilimbaris MK, Pallikaris IG, Kymionis GD, 2017. Combined transepithelial phototherapeutic keratectomy and conventional photorefractive keratectomy followed simultaneously by corneal crosslinking for keratoconus: cretan protocol plus. J. Cataract Refract. Surg43, 1257–1262
About the Doctor:
 Dr. Millette Romualdez is a Fellow of the American Academy of Optometry, Scleral Lens Society, Philippine College of Optometry and International Association of Contact Lens Educators. She has also received a Certification of Advanced Contact Lenses from the Australian College of Optometry.
Dr. Millette Romualdez is a Fellow of the American Academy of Optometry, Scleral Lens Society, Philippine College of Optometry and International Association of Contact Lens Educators. She has also received a Certification of Advanced Contact Lenses from the Australian College of Optometry.
To book an appointment for a doctor that fits keratoconus contact lenses such as scleral contact lenses, GP lenses and Kerasoft IC , contact us via 09215452389 or docmillette@goldheartoptical.com.